Our Complete Knowledgebase
Below you will find detailed how-to articles to help you get started or troubleshoot issues with Aqueduct, our teaching and learning platform.
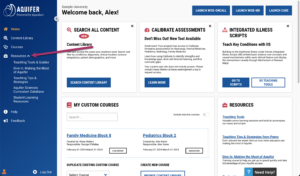
Additional Support Resources Available In-Platform
Key Resources: Inside Your Aquifer Account
Get started or optimize the way you are using Aquifer with separate cases covering how-to’s for administrators and best practices for faculty. Complete the case or cases that apply to your role to quickly get up to speed. Located on the Courses page inside your Aquifer account.
Interactive Guidance & Searchable Support
In your Aquifer account, click the “Need Help?” button to access our searchable support, complete with guided walk-throughs available for many key tasks.
Search Support Resources
Resources for:
Filter - All
Students
Educators
Administrators
Topics:
Filter - All
flipping the classroom
TBL
team-based learning
exams
assessment
reports
clinical decision-making
clinical reasoning skills
curriculum integration
educator resources
active learning modules
user management
custom course
advanced case search
course management